Olin’s healthcare symposium draws standing room only crowd
- January 28, 2019
- By Kurt Greenbaum
- 5 minute read
Every country is looking to the United States for innovation in financing and innovation in care.
—Dr. Ezekiel J. Emanuel
Some disagreed on the way to fix rising prescription drug costs. Others differed on the priority non-medical social interventions should receive in the healthcare system. Others didn’t see eye-to-eye on the medical efficacy of expensive proton beam therapy in treating cancer.
But one theme drew universal agreement in Olin Business School’s healthcare symposium, a Calhoun Lecture Series event held on January 23: The US healthcare system is broken, bloated and bound for change.
The morning-long symposium drew a standing-room-only crowd of students, alumni, local industry leaders and faculty that spilled from Emerson Auditorium into Frick Forum to hear two panel discussions, plus a keynote address from industry rock star Dr. Ezekiel J. Emanuel, whose credentials extend from private sector medicine to government policy and into medical academia at the University of Pennsylvania.
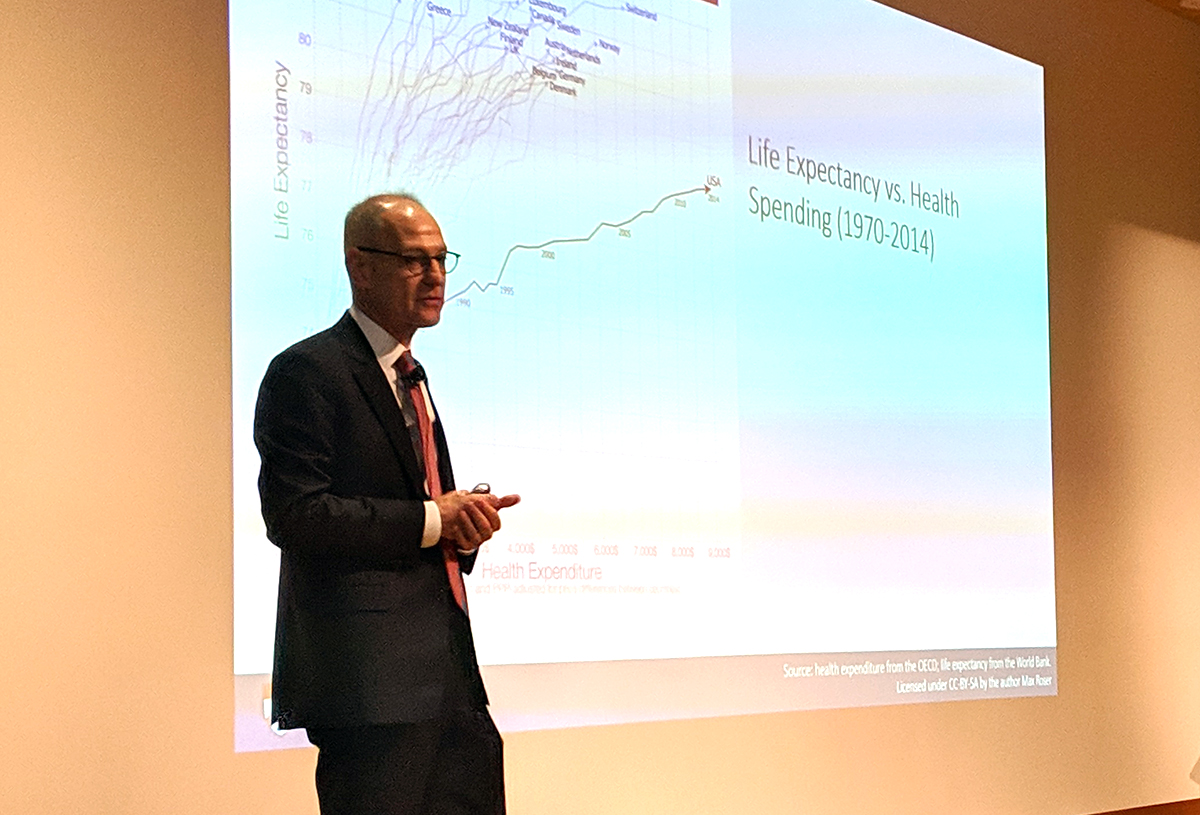
Emanuel launched his talk by noting that US spending on healthcare—$3.5 trillion in 2017—was greater than the total GDP of several major global powers, including the United Kingdom. Then he shared the “single most depressing slide about American healthcare,” graphing healthcare spending from numerous developed countries against the life expectancy of their residents.
“We are spending a huge amount of money and not getting any return on it,” Emanuel told the audience, showing how the United States has “fallen off the curve” against countries such as Japan, Switzerland and Australia, who spend considerably less on healthcare, while their residents live much longer.
Still optimistic about change
The problem, Emanuel said, is a chronic case of wasted spending on unnecessary procedures, inefficient care and “pricing failures” that reward providers for the wrong outcomes. Yet through it all, he said, “I’m wildly optimistic about the American healthcare system. And the reason is California wine.”
He referred to the 1976 “Judgment of Paris,” a first-ever blind taste test in which California vintners shocked the wine world by prevailing over French wines. The lesson: US innovators can do anything they set out to do.
“Every country is looking to the United States for innovation in financing and innovation in care,” Emanuel said. He cited four areas of focus that would move the industry in the right direction.
- Value-based payment or bundled payments. Rather than the existing “fee-for-service” model, bundled payments would put patients and insurers on the hook for a “unit of care”—e.g., a hip replacement—with the costs integrated and later divvied up among individual providers. The model would incentivize providers to better coordinate care and cut unnecessary costs.
- Deinstitutionalization and shifting care. Years ago, Emanuel said, the United States saw about 171 hospitalizations for every 1,000 patients. That’s down to about 103 in 2017. “We’ve shifted a lot of our care and we’re going to shift more of it out of the hospital,” he said, and those changes include the trend toward “minute-clinics” in drug stores and the reduced reliance on physicians in favor of nurse practitioners, physician assistants and virtual medicine.
- Chronic disease management. Eighty-six cents of every dollar spent in healthcare is spent on on chronic disease management. Emanuel cited the example of Texas’ Rio Grande Valley, where half the population is afflicted with diabetes. The community has developed specialty clinics and aggressive outreach to the community. “The key to care management is active outreach—not waiting for them to show up sick.”
- Behavioral health integration. “We have been isolating psychiatry ‘over there.’ Records are different. Billing is different. Bad, bad mistake,” Emanuel said. “You can bring down healthcare costs by treating co-morbid depression and anxiety” that accompanies many physical disorders.
Other interventions
After Emanuel’s talk, the audience heard from two separate panels, the first looking at “disruption in treatment” and the second focusing on “innovation in delivery methods” for healthcare. Below are a selection of moments from the program.
On the social impacts to health. Blake Marggraff, CEO of Epharmix, spoke about an incident involving a review of patients suffering from chronic respiratory disease. “There were some conversations that turned from, ‘Are you breathing OK?’ to ‘Sure, yes, but I’m also having trouble paying my rent this month.'”
On technology and the need to better engage with individual patients. Mike Kaplan, founder of Altos Health, spoke of working with a “company that developed software allowing physicians to reach out individually to patients. The patients were engaging in this conversation with the physician and we were able to catch things earlier—lack of return to functional status, pain issues, infections.”
On drug prices. Emanuel said government regulation was the only solution. Steve Miller, chief medical officer at Express Scripts, said it could come to that, but there are intermediate steps that could allow the market to work. “Americans will try everything before they’ll try the right thing,” he said. “I’m a big believer in market-based solutions to drug pricing. The science is spectacular; the question is, is America willing to pay these prices.”
WashU’s Michael Kinch was a bit more blunt: “The pharmaceutical industry is the most efficiently self-immolating industry I’ve ever seen,” said Kinch, associate vice chancellor and director of the Center for Research Innovation in Business at the Institute for Public Health.
On spending: “America doesn’t have a money problem, it has a waste problem,” Miller said. “Healthcare is a tax on every single product in the country. When it’s 18 percent of GDP, everything is being taxed…America wants personalized care at public health prices.”
On access to healthcare: “Only about 50 percent of Americans have a primary care physician with whom they work,” said Sandra Van Trease, group president, BJC HealthCare. “Many receive care via phone—so developing trust happens differently. Being consumer-centric in how we create access is key.”
Mike Long, CEO of Lumeris, threw down the challenge for the next generation of business school students and medical professionals. “We have such a tremendously flawed system,” he said. “I’m hoping young people commit themselves to working in healthcare because they’re mad as hell and aren’t going to take it anymore.”
Pictured above: Dr. Ezekiel J. Emanuel presenting his keynote address at Olin’s healthcare symposium on January 23. He is vice provost for global initiatives, the Diane S. Levy and Robert M. Levy University Professor and chair of the Department of Medical Ethics and Health Policy at the University of Pennsylvania.
Media inquiries
For assistance with media inquiries and to find faculty experts, please contact Washington University Marketing & Communications.
Monday–Friday, 8:30 to 5 p.m.
Sara Savat
Senior News Director, Business and Social Sciences
